



















Note that you will need either
RealPlayer
or
QuickTime
to view these files. The QuickTime files clearly show details, but are
larger and take longer to download, while the RealPlayer files are smaller
but show far less detail. The size of each file will display in the status
bar as you put the mouse over each picture, below.
The whole blood typing process is available as a RealPlayer video.
| File Size |
Running Time | ||
|---|---|---|---|
| The Whole Process | 1.86 MB | 12 min |
Or, to see a specific segment, click on a picture to view the corresponding movie.
| QuickTime | RealPlayer | ||
|---|---|---|---|
 |
No Food or Drinks | 0:30 |  |
| Because of the danger of contamination with blood, all soft drinks, candy, and food should be removed from the lab or put safely away in your bookbag before the lab begins. | |||
 |
Use Gloves When Helping | 0:19 |  |
| To reduce the danger of contamination, you should do your own blood typing. If it becomes necessary to help someone else, you must wear gloves for your own protection. | |||
 |
Antisera | 0:24 |  |
| The antisera should be at room temperature when they are used. The blue antiserum is anti-A antibodies, the yellow one is anti-B, and the “clear” one is anti-D (anti-Rh+). | |||
 |
Equipment Used | 1:16 |  |
| Insure that all equipment listed in your lab protocol is available and ready for use. | |||
 |
Marking the Slide | 0:41 |  |
| A wax pencil should be used to “divide” a slide into thirds and draw a large circle in each third. The circles should be labeled (“A,” “B,” or “D,”) and the slide should be initialed. | |||
 |
Loading the Lancet | 0:37 |  |
| The lancet should be inserted into the Autolet® and the tip guard carefully removed. After the Autolet® is “closed,” an orange finger platform should be inserted. | |||
 |
Adding Antisera to Slide | 1:15 |  |
| A drop of the appropriate antiserum should be placed just inside one edge of the appropriate circle. Care should be taken that the antisera are not cross-contaminated. | |||
 |
Sterilizing Finger | 0:24 |  |
| The appropriate finger should be sterilized with a Kimwipe® and 70% ethanol and allowed to air-dry. If you are right-handed and do not play guitar, etc., the ring finger of your left hand should be used. | |||
 |
Pricking Finger | 2:10 |  |
| Hold hand below your heart. Working quickly, lance the fleshy side of the tip on the little-finger side, place a drop of blood inside the opposite edge of each circle, then stir each with its own toothpick. | |||
 |
Rh Viewbox | 0:40 |  |
| Place your slide on the Rh viewbox to warm it, and gently rock the viewbox back and forth to help the antisera to react with any antigens present on your RBCs. | |||
 |
Proper Disposal of Trash | 1:26 |  |
| While your slide is reacting, THREE toothpicks, the lancet cover, and any paper should be properly disposed of. The orange finger platform and the lancet should be ejected into the correct containers. | |||
 |
Nothing in Trash Can | 0:27 |  |
| Lancets should never be placed into the regular trash because someone could get stuck. Lancets should only be placed in the specially-marked sharps container. | |||
 |
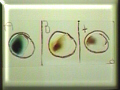
Agglutination | 0:17 |  |
| Examine your slide for agglutination. A graininess in any of the circles is a reaction that indicated that you have that blood type. Record these data in your lab notebook. | |||
 |
Slide into Bleach Solution | 0:31 |  |
| Gently place your used slide into a 10% solution of chlorine bleach to disinfect it (lab personnel will complete the process). Wearing goggles can prevent eye injury due to splashed bleach solution. | |||
 |
End-of-Day Clean-Up | 1:18 |  |
| Before you leave, make sure all blood-stained items are correctly disposed of. Other classes should be warned to consume no food in the lab room until the tabletops have been treated with bleach-water. | |||
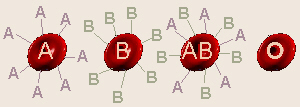 Many genes only have two alleles. An interesting exception to this (there
are others) is the human ABO blood group. The alleles are IA,
IB, and i, so the possible genotypes/phenotypes are
IAIA or IAi = type A blood,
IBIB or IBi = type B blood,
IAIB = type AB blood, and ii = type O
blood. These phenotypes are not all equally-distributed in all populations
of humans. In the U. S., about 45% of the population is type O, 42% type A,
10% type B, and only 3% type AB. However, other cultures/ethnic groups exist
in which 75% of the people are type A and 25% type 0 (no B or AB), or where
40% of the people have type B with a mixture of the other types also present.
Many genes only have two alleles. An interesting exception to this (there
are others) is the human ABO blood group. The alleles are IA,
IB, and i, so the possible genotypes/phenotypes are
IAIA or IAi = type A blood,
IBIB or IBi = type B blood,
IAIB = type AB blood, and ii = type O
blood. These phenotypes are not all equally-distributed in all populations
of humans. In the U. S., about 45% of the population is type O, 42% type A,
10% type B, and only 3% type AB. However, other cultures/ethnic groups exist
in which 75% of the people are type A and 25% type 0 (no B or AB), or where
40% of the people have type B with a mixture of the other types also present.
Rh factor is a totally separate gene with Rh+
[R] and Rh– [r] alleles [actually, that gene also has multiple
alleles, but the vast majority of people are positive or negative for one
particular allele called “D”]. In the U. S., about 85% of the population is
Rh+ [RR and Rr] and 15% Rh– [rr], thus the chances of
someone being O– [having both ii and rr] would be 45% × 15%
= 6.75%. The rarest blood type in the U. S. would be AB–, about
0.45% of the population.]
| We previously mentioned the ABO blood types. Hopefully, you recall that the possible alleles for this gene are IA, IB, and i. From this, the following genotypes and corresponding phenotypes are possible: |
| |||||||||||||||
 On the surface of all of our cells are
antigens
which are substances that our immune systems use to distinguish “me” from
a foreign invader. For the ABO blood group gene, the A and B alleles code
for production of special short-chain polysaccharides which are the antigens.
Type O is the lack of A and/or B antigens which are found on the
surface of RBCs (red blood cells). In actuality, the O allele codes
for a more simple polysaccharide that doesn’t trigger generation of antibodies,
but for our purposes, it’s kind of like there’s no O antigen. Our immune
systems are supposed to make antibodies against foreign invaders
(measles, mumps, kidney transplants, blood transplants = transfusions, etc.)
but not against “me”. Normally, someone’s immune system will not make
antibodies against any of the antigens on that person’s own cells. That’s
why, when someone needs a transplant, an attempt is made to find tissue that
matches the person’s own tissue as closely as possible. so his/her immune
system doesn’t make antibodies against the transplant and “reject” it.
On the surface of all of our cells are
antigens
which are substances that our immune systems use to distinguish “me” from
a foreign invader. For the ABO blood group gene, the A and B alleles code
for production of special short-chain polysaccharides which are the antigens.
Type O is the lack of A and/or B antigens which are found on the
surface of RBCs (red blood cells). In actuality, the O allele codes
for a more simple polysaccharide that doesn’t trigger generation of antibodies,
but for our purposes, it’s kind of like there’s no O antigen. Our immune
systems are supposed to make antibodies against foreign invaders
(measles, mumps, kidney transplants, blood transplants = transfusions, etc.)
but not against “me”. Normally, someone’s immune system will not make
antibodies against any of the antigens on that person’s own cells. That’s
why, when someone needs a transplant, an attempt is made to find tissue that
matches the person’s own tissue as closely as possible. so his/her immune
system doesn’t make antibodies against the transplant and “reject” it.
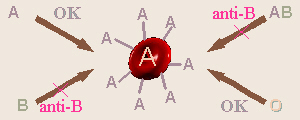
A person with type A blood can/does make anti-B antibodies so can receive blood from type A, and in an emergency, type O (type O is not used unless it is really necessary because that blood would have some anti-A and anti-B antibodies in it and could cause a problem when it mixed with the person’s blood). Type B blood can make anti-A antibodies so can receive type B (and in an emergency, type O). Type AB blood won’t make either anti-A or anti-B antibodies because it has both A and B antigens on its cells, so a person who is type AB can, in theory, receive any any other blood type (but the best idea is still to use only AB). Because of this, type AB is called the universal recipient. Type O, which has neither antigen, can make both anti-A and anti-B antibodies, thus can only receive type O. However, because, in theory, it contains no antigens to sensitize someone with types A, B, or AB blood, it can, in theory, be given to anyone and so is called the universal donor.
Rh factor is another, totally different, unrelated gene, that just happens to code for another type of cell-surface antigen that also just happens to occur on RBCs. This blood trait was named after Rhesus monkeys where it was first discovered. Actually the Rh gene has multiple alleles, but most people are + or – for the one most common “D” allele, so it’s treated as though it just has two alleles. Thus, Rh+ is the presence of this antigen (a dominant allele symbolized by R), and Rh– is, for our purposes, the absence of any antigen (a recessive allele symbolized by “r”).
Since ABO and Rh are totally separate genes, a person has to have alleles for antigens for BOTH the ABO and the Rh blood groups, so if you’re doing a genetic cross where you’re looking at both traits, you have to treat it as a dihybrid cross. For example, consider the cross IAiRr × IBiRr. The Punnett square for this cross would look like:
IAR |
IAr |
iR |
ir | |
IBR |
IAIBRR |
IAIBRr |
IBiRR |
IBiRr |
IBr |
IAIBRr |
IAIBrr |
IBiRr |
IBirr |
iR |
IAiRR |
IAiRr |
iiRR |
iiRr |
ir |
IAiRr |
IAirr |
iiRr |
iirr |
Notice the “strange” phenotype ratio of 3:1:3:1:3:1:3:1.
A special case dealing with Rh factor is that of an Rh– woman married to an Rh+ man. Recall from our discussion on testcrosses that this means, if he’s RR, all of their children will be Rh+ and if he’s Rr, half of the children will be Rh+. Since Rh– blood doesn’t have the Rh cell surface antigen, the mother can make anti-Rh+ antibodies, but needs exposure to the Rh+ antigens first to do so. When she’s pregnant with her first baby, hopefully all will be well because she probably has had no previous exposure to Rh+ blood. Blood cells don’t cross the placenta, so her blood shouldn’t be exposed to the baby’s blood and everything should be OK. As the baby is being born, due to the bleeding, etc., some of the baby’s blood will probably come into contact with hers. From this exposure, she can develop anti-Rh+ antibodies. While blood cells don’t cross the placenta, antibodies do, and normally this is a good thing: that’s how a newborn baby gets its immunity for the first few weeks.
However, if this mother becomes pregnant again, anti-Rh+ antibodies will probably go into baby #2’s blood, and if baby #2 is Rh+, these antibodies can react with his/her blood, making it agglutinate. This is when the blood cells clump together due to an antigen-antibody interaction, which is a major problem if it happens in a baby’s body (the baby might need to be given a total transfusion at birth). To prevent this from happening, after the birth of baby #1, the mother is given a shot called Rhogam which contains the very antibodies they’re trying to prevent her body from forming! The idea is that if the mother has antibodies (which are “only” proteins) already floating around in her blood, her immune system won’t get “turned on” and learn how to make antibodies. Antibodies are produced by white blood cells (WBCs) only if/after they have been exposed to an antigen and only if a lot of other WBCs aren’t already making that antibody. Presence of a lot of a particular antibody would indicate that other cells are manufacturing it, so by giving her Rhogam, it tricks her WBCs into “thinking” that “somebody else” is making antibodies so “I don’t have to.” Since antibodies are only protein, they don’t last forever and eventually go away. If her WBCs never get turned on to make more, no more will be made, so by the time baby #2 comes along things should be OK. For this reason, it is also important for an Rh– woman to get Rhogam after a miscarriage or an abortion.
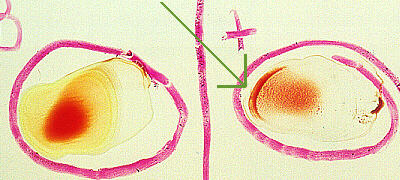
Agglutination
When doing blood typing, a drop of each of anti-A, anti-B, and anti-D
(= anti-Rh+) antisera (antibodies) is placed into its own circle
on a glass slide. Then a drop of the person’s blood is added to each drop of
antiserum. If the mixture turns “grainy,” that indicates that agglutination
has taken place, therefore the person has/is that blood type. In this photo,
the person’s blood reacted with the anti-D antiserum, thereby indicating that
the person is Rh+.
Make sure you have all of the following in your lab notebook: