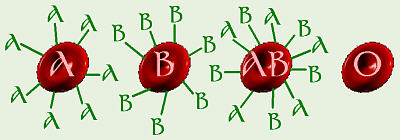
Blood Cell Antigens
We previously mentioned the ABO blood types. Hopefully, you recall that the possible alleles for this gene are IA, IB, and i. From this, the following genotypes and corresponding phenotypes are possible:
Blood Cell Antigens
| Genotype | Phenotype | |
|---|---|---|
| IAIA IAi |
} | type A |
| IBIB IBi |
} | type B |
| IAIB | type AB | |
| ii | type O | |
On the surface of all of our cells are antigens which are substances that our immune systems use to distinguish “me” from a foreign invader. For the ABO blood group gene, the A and B alleles code for production of special short-chain polysaccharides which are the antigens. Type O is the lack of A and/or B antigens which are found on the surface of RBCs (red blood cells). In actuality, the O allele codes for a more simple polysaccharide that doesn’t trigger generation of antibodies, but for our purposes, it’s kind of like there’s no O antigen. Our immune systems are supposed to make antibodies against foreign invaders (measles, mumps, kidney transplants, blood transplants = transfusions, etc.) but not against “me”. Normally, someone’s immune system will not make antibodies against any of the antigens on that person’s own cells. That’s why, when someone needs a transplant, an attempt is made to find tissue that matches the person’s own tissue as closely as possible. so his/her immune system doesn’t make antibodies against the transplant and “reject” it.

A person with type A blood can/does make anti-B antibodies so can receive blood from type A, and in an emergency, type O (type O is not used unless it is really necessary because that blood would have some anti-A and anti-B antibodies in it and could cause a problem when it mixed with the person’s blood). Type B blood can make anti-A antibodies so can receive type B (and in an emergency, type O). Type AB blood won’t make either anti-A or anti-B antibodies because it has both A and B antigens on its cells, so a person who is type AB can, in theory, receive any any other blood type (but the best idea is still to use only AB). Because of this, type AB is called the universal recipient. Type O, which has neither antigen, can make both anti-A and anti-B antibodies, thus can only receive type O. However, because, in theory, it contains no antigens to sensitize someone with types A, B, or AB blood, it can, in theory, be given to anyone and so is called the universal donor.
Rh factor is another, totally different, unrelated gene, that just happens to code for another type of cell-surface antigen that also just happens to occur on RBCs. This blood trait was named after Rhesus monkeys where it was first discovered. Actually the Rh gene has multiple alleles, but most people are + or – for the one most common “D” allele, so it’s treated as though it just has two alleles. Thus, Rh+ is the presence of this D antigen (a dominant allele symbolized by R), and Rh– is, for our purposes, the absence of any antigen (a recessive allele symbolized by “r”).
A person has alleles for antigens for BOTH the ABO and
the Rh blood groups, so if you’re doing a genetic cross where you’re looking
at both traits, you have to treat it as a dihybrid cross. For example,
consider the cross IAiRr × IBiRr. The Punnett square
for this cross would look like:
| IAR | IAr | iR | ir | |
| IBR | IAIBRR | IAIBRr | IBiRR | IBiRr |
| IBr | IAIBRr | IAIBrr | IBiRr | IBirr |
| iR | IAiRR | IAiRr | iiRR | iiRr |
| ir | IAiRr | IAirr | iiRr | iirr |
Notice the “strange” phenotype ratio of 3:1:3:1:3:1:3:1.
A special case dealing with Rh factor is that of an Rh– woman married to an Rh+ man. Recall from our discussion on testcrosses that this means, if he’s RR, all of their children will be Rh+ and if he’s Rr, half of the children will be Rh+. Since Rh– blood doesn’t have the Rh cell surface antigen, the mother can make anti-Rh+ antibodies, but needs exposure to the Rh+ antigens first to do so. When she’s pregnant with her first baby, hopefully all will be well because she probably has had no previous exposure to Rh+ blood. Blood cells don’t cross the placenta, so her blood shouldn’t be exposed to the baby’s blood and everything should be OK. As the baby is being born, due to the bleeding, etc., some of the baby’s blood will probably come into contact with hers. From this exposure, she can develop anti-Rh+ antibodies. While blood cells don’t cross the placenta, antibodies do, and normally this is a good thing: that’s how a newborn baby gets its immunity for the first few weeks.
However, if this mother becomes pregnant again, anti-Rh+ antibodies will probably go into baby #2’s blood, and if baby #2 is Rh+, these antibodies can react with his/her blood, making it agglutinate. This is when the blood cells clump together due to an antigen-antibody interaction, which is a major problem if it happens in a baby’s body (the baby might need to be given a total transfusion at birth). To prevent this from happening, after the birth of baby #1, the mother is given a shot called Rhogam which contains the very antibodies they’re trying to prevent her body from forming! The idea is that if the mother has antibodies (which are “only” proteins) already floating around in her blood, her immune system won’t get “turned on” and learn how to make antibodies. Antibodies are produced by white blood cells (WBCs) only if/after they have been exposed to an antigen and only if a lot of other WBCs aren’t already making that antibody. Presence of a lot of a particular antibody would indicate that other cells are manufacturing it, so by giving her Rhogam, it tricks her WBCs into “thinking” that “somebody else” is making antibodies so “I don’t have to.” Since antibodies are only protein, they don’t last forever and eventually go away. If her WBCs never get turned on to make more, no more will be made, so by the time baby #2 comes along things should be OK. For this reason, it is also important for an Rh– woman to get Rhogam after a miscarriage or an abortion.
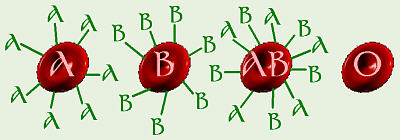
Agglutination
When doing blood typing, a drop of each of anti-A, anti-B, and anti-D (=
anti-Rh+) antisera (antibodies) is placed into its own circle on a
glass slide. Then a drop of the person’s blood is added to each drop of
antiserum. If the mixture turns “grainy,” that indicates that agglutination
has taken place, therefore the person has/is that blood type. In this photo,
the person’s blood reacted with the anti-D antiserum, thereby indicating that
the person is Rh+.

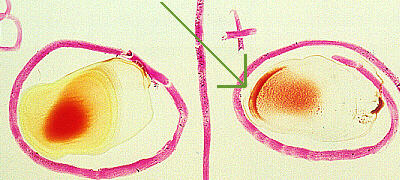
Normal RBC

Sickled RBC
Sickle-cell anemia is a mutation of only one nucleotide in the gene
that codes for hemoglobin. This is a recessive trait (not really – see
following explanation – but for our purposes, it’s easier to think of it
that way), so S = normal hemoglobin and s = sickle-cell
hemoglobin. SS is a normal person while ss has sickle-cell
anemia. Many people with ss die from complications associated with the
abnormally-shaped RBCs that result from the sickle-cell anemia. Sickle-cell
is common among African Blacks from areas where there’s a lot of
malaria.
Malaria is caused by a parasite (Kingdom Protista: Plasmodium vivax)
that invades RBCs and lives best in normal RBCs, thus people who are SS are
more likely to die from malaria. When the parasite invades a RBC with
sickle-cell hemoglobin, the cell sickles in response and then is destroyed
by the body (and the parasite along with it). The parasites have a harder
time multiplying and infecting people who are ss, so ss is fairly resistant
to malaria (but dies from sickle-cell). The heterozygote (Ss) exhibits
incomplete dominance or codominance: the S allele codes for normal
hemoglobin and the s allele codes for sickle-cell hemoglobin, so the person
has some of each. Normally the person is OK, but under stress, some RBCs
may sickle (don’t send that person up to Denver to run a marathon race).

A photo, taken by Dr. Fankhauser, of a prepared slide
of blood cells infected with Plasmodium vivax
The heterozygote is somewhat more resistant to malaria because the parasites
frequently are destroyed when they stress the RBCs enough to make them sickle.
The fact that SS people die from malaria and ss people die from sickle-cell
while Ss live keeps what otherwise would be a “bad” allele (sickle-cell) in
the population. Normally, most “bad” recessive traits eventually breed out
of the population as the homozygous dominant and the heterozygote take over
but with the sickle-cell allele, if Ss are the people surviving and
reproducing, remember that half of their children would also be Ss (and
the other half – SS and ss – die from one reason or the other).
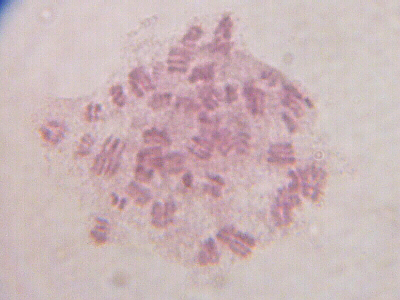
A photo of human white blood cells that were specially cultured,
treated with Colcemid, and stained to show chromosomes.
When we’re talking about all of a person’s genes/chromosomes, we refer to that
person’s genome, which means all of an organism’s genetic
material. To study this in humans, a
karyotype
is done. This involves obtaining blood cells, growing them in tissue culture
for a few days, staining the cells, photographing the chromosomes in the cells,
cutting out chromosomes from the picture, and lining them up in pairs by size
(#1 to 23). Note that pair #23 consists of unmatched XY, which usually
makes the person male, or matched XX, which usually makes the person female.
The source of blood for children and adults is a finger prick. For an
unborn baby,
amniocentesis
is done. Karyotyping is used to screen for an abnormal number of chromosomes
(for example, three of chromosome #21, which produces Down Syndrome).
Remember when we were discussing meiosis, it was mentioned that meiosis in human females is unusual in that it starts during embryonic development, then stops in about prophase I. Once a female reaches puberty, normally one “egg” per cycle goes farther through the process of meiosis. This means that the “eggs” in a 40-year-old woman have been sitting around “waiting” for twice as long as those in a 20-year-old woman, and sometimes they “forget” how to divide properly. Sometimes, both homologous chromosomes in a pair will be pulled to one pole of the cell, while the other end gets none from that pair. Nondisjunction is the non-separation of homologous chromosomes during meiosis, and after fertilization, results in the condition of trisomy for that particular chromosome: trisomy 21 produces Down Syndrome. A more general term for possessing an abnormal number of chromosomes is aneuploidy, having extra copies or not enough of certain chromosome(s).
Statistically, it has been shown that there is a correlation between maternal age and chances of having a baby with Down Syndrome. At age 40, a woman’s chances of having a baby with Down Syndrome are about 1/100, and at 45 about 3/100. That’s why doctors want to do amniocentesis on older women. (Interestingly, several years ago when a doctor wanted to do some testing on me, for something totally unrelated, her advice to me was basically, “Don’t worry about it, the chances are only about 20/100 that there might be a problem, so there probably won’t be,” — and there wasn’t). Also, the risk of complications from amniocentesis, including possible premature labor and expulsion of the baby, is about 1/100 and the risk of complications from chorionic villi sampling is about 2/100. Thus, for an “older” mother, the chances of amniocentesis or chorionic villi sampling causing a problem, including possible death of the baby, are roughly equal to the chances of having a baby with Down Syndrome, while statistically, a “younger” mother has far less chance of a Down Syndrome baby. Is it worth it? It is also true that the father’s age can affect sperm production thus also influences chances of Down Syndrome too (caused by nondisjunction in meiosis during sperm production).
Because amniocentesis typically can’t be done before about the fourth to fifth month of pregnancy, more doctors now are trying chorionic villi sampling because it can be done earlier. However, this process is more invasive: the mucus plug in the woman’s cervix that seals off her uterus to protect the unborn baby from infection is removed, and instruments are inserted, around (hopefully) the baby, to take a sample of the placenta. The results can be confusing if the technician gets some of the mother’s tissue as well as the baby’s. These procedures are basically used to decide whether to “follow up” with abortion. Because there have been a number of lawsuits (for things such as “wrongful birth” — like, getting pregnant was the doctor’s fault?) against doctors in recent history, most doctors will strongly urge women over 35 to have one or the other of these tests done. For a couple who feel comfortable with the possibility of abortion, these tests can give them some information about their baby’s genetics that could possibly influence their decision, but a couple who are morally opposed to abortion might not wish to risk having one of these procedures performed to gain information that will be more easily observed in a few months when the baby is born. Recently, various insurance companies have suggested making amniocentesis for women over 35 mandatory because it’s cheaper for them to pay for an abortion than medical care for the child for the rest of his/her life, thereby reducing the value of the life of the child to merely the cost of medical care for him/her. What’s your opinion: if a couple has serious moral/religious objections to abortion, do you think their health insurance provider should make it mandatory that they must have amniocentesis and possibly an abortion performed?
Nondisjunction also occurs in the sex chromosomes, resulting in conditions such as XO (Turner’s) and XXY (Klinefelter’s). We see nondisjunction of sex chromosomes and chromosome #21 more often because those affect the person LESS, so the person is more likely to live. Most other aneuploids result in death before birth and miscarriage, or death shortly after birth. Sometimes it’s not a whole chromosome, but a big piece, that’s missing, or perhaps a big piece breaks off and attaches to another chromosome before meiosis occurs. Some forms of Down syndrome involve an extra piece of #21 stuck on another chromosome. This is called translocation. There are other possible effects of translocations. For example, if in a man’s testes, just prior to sperm formation, a piece of his Y chromosome, including some of the genes that code for male traits, gets translocated to his X chromosome, and later, a sperm containing that modified X chromosome is the one that fertilizes an egg, the resulting baby would be a boy who has XX chromosomes.
There are a number of other genetic disorders that “frequently” affect humans. The alleles for these disorders are not equally prevalent in all ethnic groups. Some recessive disorders include cystic fibrosis, which causes an abnormally large amount of mucus in the lungs and is most common among Caucasians (whites); Tay Sachs, which is a neurological disorder and is most common among eastern European Jewish people; and sickle-cell, which was just discussed and is most prevalent in African Blacks. There are also some disorders that are dominant alleles, so if someone is a heterozygote, (s)he will have that trait. Since about the only way someone could be homozygous dominant would be if both parents passed on that allele, most people who have these disorders are heterozygotes. There is, thus, a 50% chance they will pass these alleles to their children, assuming the trait is such that they live long enough to reproduce. One such dominant trait is achondroplasia. In this disorder, if an individual would be AA, that baby would die before birth and the mother would have a miscarriage. An individual with genotype Aa would be a dwarf, and aa is normal height.
Huntington’s disease is another dominant disorder that is a progressive deterioration of the person’s nervous system that starts in middle age, after the person may already have had children. Because it’s a dominant allele, if a child gets that allele, (s)he will have the disorder (BUT... the severity and progression of the symptoms varies considerably from person to person), thus some couples might choose to not have children if they knew one of them had the allele. There is a genetic test available to tell if a person has Huntington’s, so if a person chose to have this test, a couple could make that decision. Because Huntington’s destroys the nervous system, the person gradually loses control of body and brain functions until the nerves won’t control his/her heart and breathing, then dies. Thus, if a person chose to have the test done, (s)he would know ahead of time that in a few years (s)he could gradually deteriorate into a helpless state. Each time (s)he dropped something or forgot something, (s)he might be tormented by the idea that this was a sign that the disease was beginning. Thus, some people choose to not have the test because the mental anguish of knowing what lies ahead is “too much.” Woody Guthrie, who wrote “This Land is Your Land” inherited Huntington’s from his mother and died of Huntington’s in 1967. His son Arlo Guthrie (who wrote “Alice’s Restaurant”), is now a grandfather and has not shown any signs of the disease, but several of Woody’s other children have died from Huntington’s. What’s your opinion: if you were in that situation, do you think you’d want to have the test done?
Here’s an hypothetical situation (borrowed from BSCS):
suppose a big-name company is looking for a very knowledgeable person to work
on research and development for an important project that promises to make
lots of money for the corporation. Because of this, they’re looking for
someone who will stay with the company for 10 or 20 years. In return,
they’re willing to pay quite a large salary for this position. The top
candidate for the position is a person who is 35, and who has a family
history of Huntington’s disease. The #2 candidate’s qualifications are
considerably less. If the company hires their #1 choice, there’s a 50%
chance that in as few as 5 years, they may be in a position where they’re
paying for disability insurance for this person who is now institutionalized
and can no longer work, plus having to go through the whole process of
hiring someone else to take over in the middle of the project, which could
be financially very expensive for them, plus a big set-back due to lack
of someone working on the project as the person’s health is starting to
decline, during the interview period, and while the new person is “getting
up to speed.” Because of this, they’d like to require the candidate to
undergo genetic testing to determine if he has Huntington’s and not hire him
if he does, but he doesn’t want to know ahead of time if he had the disease,
so he does not want to have the test done. This test is not a part of what
the company normally requires for all new employees.
What’s your opinion:
Should the company mandate this test for this particular person against his
wishes? Should they deny him employment if he refuses to have the test
done? What if they don’t hire him, and it turns out his symptoms show up
very late in life and are very mild and slow-progressing, so he could have
made a significant contribution to the company? What if they decide to
hire #2, who does a poor job and they don’t make as much money as they had
hoped? What if whoever they hire gets killed in a car accident a year
later?
Genetic counselling is available to help couples with family histories of genetic problems decide whether to have a baby. Based on things like construction of a family pedigree for the gene in question and possibly some genetic testing, if available, the couple is given information and advised of the chances any children they might have will have that disorder. Once a woman is pregnant, there are a variety of prenatal tests that can give them information about the genetic condition of their baby before (s)he is born. However, many of these tests are not without risks. Ammiocentesis and chorionic villi sampling have already been mentioned. While the book says ultrasound is safe, I’ve heard it suggested lately that the number of times this is done be limited because they just aren’t sure if it really is as safe as it seems. Ultrasound is a non-invasive technique in which very high pitched sound is bounced off the baby, mostly to check his/her size. The thing is, most of the conditions that could be diagnosed via these tests are things that cannot be treated prenatally, in utero.
There are other times when genetic testing and counselling may be useful in weighing the “pros” and “cons” of a situation. Several years ago, I had a student whose mother and several other relatives had died from breast cancer. She was tested for and found out that she had “the breast cancer gene.” She said, “I want to be here for my children and grandchildren,” and made the decision to have a prophylactic double mastectomy and reconstructive surgery. More recently, a famous actress has been in the news for making a similar decision.
The Web site Online Mendelian Inheritance in Man is an excellent source of information on human genes.
Interestingly, some “apparently” genetic disorders may be caused by viruses. Some viruses can insert their genes permanently into our cells. Herpes viruses like chickenpox and cold sores, mononucleosis, AIDS, and some others that cause cancer do this. Cervical cancer has been linked to prior infection with genital warts (human papilloma virus, HPV). While some kinds of cancer have been linked to genetic causes (for example, retinoblastoma, a kind of cancer of the eyes, as well as some kinds of breast cancer), others to viruses, (the HPV-cervical cancer connection just mentioned), and still others to environmental factors (smoking and lung cancer), for many kinds of cancer, there is no obvious “cause.”
Cancer cells are genetically different than normal cells. They lack the normal controls on cell division. Recall from the mitosis Web page the “Hayflick Limit” — normal cells can do mitosis about 20 to 50 times, then die, whereas cancer cells are not subject to that limit, and continue to multiply “forever.” Whereas normal cells stay within the organ/tissue of which they are a part, cancer cells can spread to other areas of the body. In tissue culture, normal cells will grow a layer that is one cell thick on the top of the culture medium and stop multiplying when they’re touching and all the available space is filled, whereas cancer cells will continue to multiply throughout the culture medium until they run out of food. As mentioned on the mitosis Web page, all of the HeLa cells that researchers are using for a wide variety of testing purposes all came from one small sample of Henrietta Lacks’ cervical cancer cells, collected back in 1951, over 60 years ago! While she would be in her 90s if she was still alive, now, the commercially available HeLa cells show no signs of stopping. In her body, the cells that were not removed “took over,” metastasising to other areas of her body and wrapping around and into various body organs until those were no longer able to function.
Modern cancer treatment has come a long way since 1951. Back then the main treatments that were used were radium and x-rays. Radium was discovered by and probably also the cause of death of Marie Curie — it’s radioactive and causes radiation burns and mutations in healthy tissue when it was used to kill cancer cells. Henrietta Lacks had her cervix packed with radium and temporarily sewn shut. She and numerous other “victims” of x-ray treatment have experienced burns, sometimes severe, and scarring in healthy tissue that was “zapped” along with the cancer. Yet, many of those treatments were unsuccessful, and people just got worse and died: pain and bodily damage from the cancer was compounded by pain and bodily damage from the treatment. Some of the ways of treating cancer, now, include:
Occasionally, a normal cell in someone’s body may mutate, may turn into a cancer cell, but normally, a healthy immune system then no longer recognizes the cancer cell as part of “me” and destroys it. However, if a person’s immune system gets stressed and run-down, that cancer cell might have a chance to reproduce, until it forms a large enough tumor that the immune system just can’t destroy it all. There are a number of things we can do to help strengthen our immune systems and decrease our chances of getting cancer. Things to avoid include tobacco/smoking, a high-fat diet (maybe...), a high-sugar diet, synthetic estrogen pills, x-rays, ultraviolet light from tanning beds and the sun, pollutants like asbestos, etc., and a variety of drugs and chemicals known to be carcinogenic. Things we can do to help strengthen our immune systems especially include eating a high fiber diet; vitamins A, C, E, and beta carotene (found in dark green, leafy veggies); foods like garlic, kale, and broccoli; and antioxidant minerals like selenium and zinc.
One of the books I read a couple years ago pointed out that, now, many kinds of cancer, if caught early enough that they’re still treatable, are analogous to type II diabetes. Both the diabetes and the cancer, if untreated, can lead to death. Both, if treated in an appropriate manner, can be kept under control so the person can lead a fairly normal life. That’s good news considering that, in this country, we’re at a point where, statistically, one out of every two people — half of the population — will be diagnosed with some form of cancer at some point in their lives.
Suppose there was some gene on the DNA:
| TAC | - | CCA | - | GGC | - | GCT | - | GAA | - | TCA | - | TGC | - | CCA | - | AGC | - | ACT |
| AUG | - | GGU | - | CCG | - | CGA | - | CUU | - | AGU | - | ACG | - | GGU | - | UCG | - | UGA |
| start | - | gly | - | pro | - | arg | - | leu | - | ser | - | thr | - | gly | - | ser | - | stop |
| TAC | - | CCA | - | GGC | - | GCT | - | GAT | - | CAT | - | GCC | - | CAA | - | GCA | - | CT? |
| start | - | gly | - | pro | - | arg | - | leu | - | val | - | arg | - | val | - | arg | - | ??? |
| TAC | - | CCA | - | GGC | - | GCT | - | ATC | - | ATG | - | CCC | - | AAG | - | CAC | - | T?? |
| start | - | gly | - | pro | - | arg | - | stop | - | (try) | - | (gly) | - | (phe) | - | (val) | - | ??? |
| TAC | - | CCA | - | GGC | - | GCT | - | TCA | - | TGC | - | CCA | - | AGC | - | ACT |
| start | - | gly | - | pro | - | arg | - | ser | - | thr | - | gly | - | ser | - | stop |
| TAC | - | CCA | - | GGC | - | GCT | - | GCA | - | TGC | - | CCA | - | AGC | - | ACT |
| start | - | gly | - | pro | - | arg | - | arg | - | thr | - | gly | - | ser | - | stop |
| TAC | - | CCA | - | GGC | - | GCT | - | GCA | - | ATC | - | ATG | - | CCC | - | AAG | - | CAC | - | T?? |
| start | - | gly | - | pro | - | arg | - | arg | - | stop | - | (try) | - | (gly) | - | (phe) | - | (val) | - | ??? |
| TAC | - | CCA | - | GGC | - | GCT | - | GAA | - | TTT | - | TCA | - | TGC | - | CCA | - | AGC | - | ACT |
| start | - | gly | - | pro | - | arg | - | leu | - | lys | - | ser | - | thr | - | gly | - | ser | - | stop |
| TAC | - | CCA | - | GGC | - | GCT | - | GAT | - | TTA | - | TCA | - | TGC | - | CCA | - | AGC | - | ACT |
| start | - | gly | - | pro | - | arg | - | leu | - | asn | - | ser | - | thr | - | gly | - | ser | - | stop |
We know that some birth defects are genetic, and some are related to substances to which the unborn child has been exposed prenatally. Substances such as ethanol, drugs such as thalidomide, and viruses such as German measles all are known to cause birth defects. Genetic conditions such as cystic fibrosis and PKU also affect newborns.
There are some things a couple can do to help guard the health and proper development of an unborn child. Folacin, one of the B vitamins, can help prevent “neural tube defects” — things like spinal bifida — when adequate amounts are present in the diets of both parents prior to conception and in the mother’s diet while she is pregnant, especially during the first three months when all the baby’s organs are forming. Avoiding alcohol and tobacco smoke (including side-stream smoke) during pregnancy can also help. If you’ve ever been to an x-ray room in a hospital, they all have signs posted that say something to the effect of, “If you think you might be pregnant, let us know before you get x-rays.” That’s because x-rays are mutagenic and teratogenic (tera, terato = a wonder, a monster), that is, they cause birth defects. Because baby girls are born with all the precursor egg cells they will ever have, and those are suspended in mid-meiosis until ovulation and fertilization (and are vulnerable to harm by x-rays: the more x-rays, the more harm), it would be a good idea if girls and women of all ages avoid gettin x-rays, especially abdominal x-rays, unless it is absolutely, positively necessary to do so. Since sperm production in men is ongoing, conventional medical thinking says this shouldn’t be as much of a problem for men, but why take a chance if you don’t have to? Both potential parents should eat a healthy diet from before they try to conceive a baby so that the sperm and egg which form that baby are as well-nourished and healthy as possible at the time of fertilization. For a new, developing baby, the first three months, the first trimester is the most critical time, because that’s when all the organs are forming (what occurs during the second and third trimesters is mostly growth of those organs), but usually, the mother doesn’t even find out that she’s pregnant until perhaps two out of those three months have passed. Thus it is critically important for her to eat a healthy diet and avoid alcohol, smoke, etc., during those first couple months when she doesn’t even know, yet, that she’s pregnant.
Our society is wrestling with a number of ethical issues tied to our modern knowledge of genetics. As citizens and taxpayers, you will be called upon to help set guidelines and legislation to direct what we as a country do with the knowledge of genetics we possess. For further information, please read Dr. Fankhauser’s Genetic Engineering Web page.
Adler, Elizabeth M. 2005. Living with Lymphoma: A Patient’s Guide. Johns Hopkins Univ. Press. Baltimore, MD.
Borror, Donald J. 1960. Dictionary of Root Words and Combining Forms. Mayfield Publ. Co.
Campbell, Neil A., Lawrence G. Mitchell, Jane B. Reece. 1999. Biology, 5th Ed. Benjamin/Cummings Publ. Co., Inc. Menlo Park, CA. (plus earlier editions)
Campbell, Neil A., Lawrence G. Mitchell, Jane B. Reece. 1999. Biology: Concepts and Connections, 3rd Ed. Benjamin/Cummings Publ. Co., Inc. Menlo Park, CA. (plus earlier editions)
Schlessel Harpham, Wendy. 2003. Diagnosis: Cancer. W. W. Norton & Co. New York.
Marchuk, William N. 1992. A Life Science Lexicon. Wm. C. Brown Publishers, Dubuque, IA.
Copyright © 1996 by J. Stein Carter. All rights reserved.