Reproductive Physiology, Conception, Prenatal Development
Background Information:
The reproductive cycles of sexually-reproducing animals are
influenced by a number of hormones, including follicle-stimulating hormone,
leutinizing hormone, estrogen, testosterone, and progesterone, produced by
the animals’ bodies. Additionally, reproductive cycles are influenced by
environmental factors such as day length. Since the hormone melatonin
is only secreted in the dark, animals’ bodies produce more melatonin in
winter months when there is less daylight. Melatonin (or lack thereof)
produces a number of physiological changes, including regulation of fertility
in many species. In humans, melatonin levels drop 75% just before puberty,
and it has been noted that blind girls whose brains/pineal glands do not
receive light from their eyes have delayed onset of puberty. In many other
species, melatonin controls sexual receptivity. For example, ewes only are
receptive in fall/winter so the lambs will be born in spring and have all
summer to grow. Typically, special sex pheromones are emitted to
convey information about receptivity to members of the opposite sex or to
regulate sexual cycles of other members of the same species.
Sperm production in males is under the control of
follicle-stimulating hormone (FSH) and leutinizing hormone
(LH). LH stimulates production of androgens (including testosterone)
by the testes, while FSH stimulates the testes to produce sperm. As in
females, production of FSH and LH are under the control of gonadotropin
releasing hormone (GnRH) produced by the hypothalamus. Via a negative
feedback loop, androgens control levels of GnRH, FSH, and LH. Additionally,
androgens are responsible for development of the male reproductive organs
during embryonic development, development of secondary sexual characteristics
(beard, deeper voice) and behaviors (singing in birds), and production of
sperm. Also via negative feedback loops, FSH and LH control production of
GnRH. In human males, it appears that blood levels of all these hormones
remain fairly constant, but in males of many other mammal species, blood
levels of these hormones vary seasonally (hinting at involvement of melatonin
in some way).

Billy Goat
Thus, in a number of species of mammals, such as goats, deer, camels, and
sheep (and Star Trek Vulcans), due to environmental and hormonal cues, the
male periodically goes into
rut,
a periodic sexual excitement in the male that is analogous to estrous in the
female. Billy goats (bucks) in rut stink worse that they do at other times.
Buck deer are more likely to use their antlers to engage in sexual
competition with other males. People who work with camels know that male
camels in rut become more unpredictable, meaner than usual, and harder to
work with and control.
In most species of mammals, the female has either an
estrous cycle
or a
menstrual cycle.
An estrous cycle is also called “being in heat” because the female’s body
temperature rises a little. However, more pronounced than changes in
temperature are noticable behavioral changes. If the female does not become
pregnant, the endometrium is reabsorbed and (usually) there is no
“bleeding”. In species in which the female has a menstrual cycle, the
unused endometrium is shed and voided from the body as the menses or
period or menstrual flow. Note that while this term was derived in the
context of human females who happen to cycle in about the same length of time
as a lunar month, it is also applied to other species whose cycles are not
one month long. Most other species have cycles that are shorter or longer
than a month, and in some species, the timing of ovulation and female
receptivity is so tied to environmental cues (light, temperature, etc.) that
they only cycle and mate at one or two specific times of the year. Human
females are somewhat unusual because the females of most species are only
receptive around the time of ovulation (release of a fertile egg). A human
female is more receptive around the time of ovulation, but that is not the
only time she is receptive. Human females generally are receptive to sexual
activity throughout their cycles.
Human Pheromones:
The average menstrual cycle in humans ranges about 20 to 40
days in length, with a statistical average of about 28 to 29 days. Some
women experience regular cycles, while others are quite irregular. Much is
understood about the hormones involved in the female cycle, but we are only
beginning to understand the role of pheromones. It is well-known that
the cycles of college women living in a dorm situation frequently adjust such
that many of the women “have their periods” at the same time as each other.
It has been shown experimentally that when perspiration from one woman is
dissolved in alcohol and applied above the upper lip of other females
(several times a week), their cycles all adjust to coincide with hers.
There is also experimental evidence that frequent exposure (several times a
week) to male perspiration (therefore, pheromones) can regulate a female’s
cycle, causing irregular, short, or long cycles to become more regular and
closer to the 28 to 29 day average. This would make sense evolutionarily
because it would increase a woman’s chances of conceiving if she was in a
situation where she had frequent contact with a stable, supportive mate who
could provide her and her child with enough food to survive (at a time when
she would be more vulnerable and less able to gather food herself, yet need
more than usual).
An interesting study on human pheromones was done in
Switzerland a number of years ago. The major histocompatibility complex
(MHC), which has to do with what antigens each person has on his/her
cells, and thus how similar or dissimilar people are, of each person in a
group of men and in a group of women was determined. Each of the men was
given a clean t-shirt and asked to sleep in it for two nights. The t-shirts
were returned to the research facility where each was placed into its own
plastic bag in its own cardboard box with a “smell hole” in the top. The
women were asked to smell each t-shirt and rank them based on which smelled
the least or most “bad” to them. Surprisingly, some of the women actually
liked the smell of some of the “stinky” t-shirts. When t-shirt preferences
were compared with each person’s MHC profile, the results showed that women
prefer the men whose MHC profile is the most different from theirs. That and
other subsequent studies showed that, in contrast, pregnant women
preferred the smell of males whose MHC profiles were the most similar
to their own. When related to success of a potential pregnancy, these data
made a lot of sense: it is known that part of the successful retention of a
pregnancy is due to bearing a baby whose genetic make-up is significantly
different from the mother’s, whereas a baby whose genetic make-up is more
similar to hers is more likely to be miscarried. Thus, one way to increase
the chances of a successful pregnancy is if the baby’s father is considerably
genetically different from the mother, and as shown in this study, that is
unconsciously “advertized” by the man’s pheromones. Once a woman is pregnant
and thus, might not be able to fend for herself in the wild and hunt her own
food, the presence of closely-related family members to provide for her and
her baby would be advantageous, hence the pregnant women’s preferences for
men who “smelled” the most like themselves (had more similar MHC profiles).
Subsequent experiments have taken this one step farther: similar studies were
done using women on “the pill.” Birth-control pills are a mixture of
hormones that mimics the hormones in a woman’s body during pregnancy, in
order to supress ovulation. Thus, as might be expected, results of these
subsequent studies showed that women taking birth-control pills preferred the
scent of men whose MHC profiles were more similar to their own. Those
results have some pretty important implications for our society. Unmarried
women who are sexually active and thus on “the pill” are sexually attracted
to men who “smell” very similar to themselves. So, suppose one of these
women falls in love, and she and her partner get married, and then later
decide to have children, so she goes off her birth-control pills. Suddenly,
now that her body no longer “thinks” she’s pregnant, her mate preferences
drastically change and she is no longer attracted to her husband! A number
of people have suggested that the widespread, casual use of birth-control
pills in our society may be intimately related to our divorce rate, and that
to help increase the chances of both a successful marriage and successful
retention of any resulting pregnancies, a woman would do well to avoid
birth-control pills.
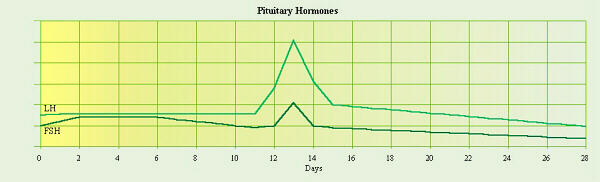
Female Cycle:
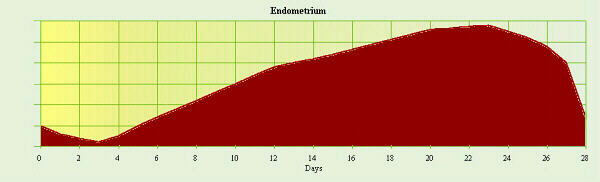
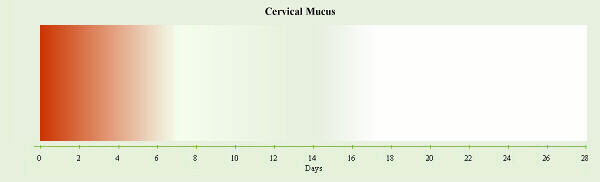
By convention, the first day of a woman’s period is considered
to be day 1 of her cycle. The first 3 to 7 days are generally the
menstrual flow phase, and during this time, all hormones involved are
at low levels. There are five hormones involved in controlling the female
cycle. These are gonadotropin releasing hormone (GnRH) secreted by
the hypothalamus, follicle-stimulating hormone (FSH) and
lutenizing hormone (LH) secreted by the pituitary gland, and
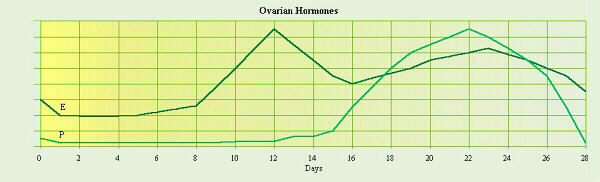
estrogen and progesterone secreted by the ovaries. The
following diagrams and explanation show how levels of these hormones and the
changes they induce vary throughout a woman’s cycle.
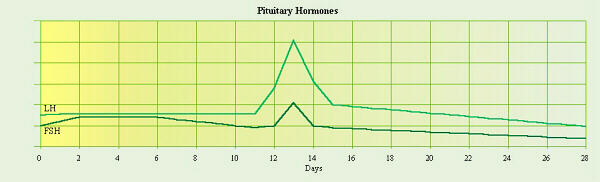
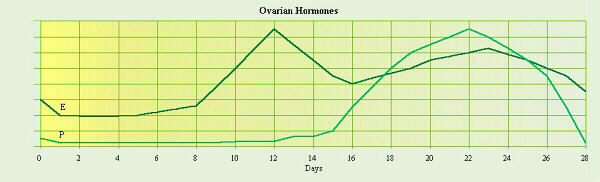
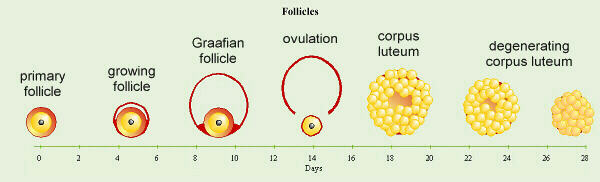
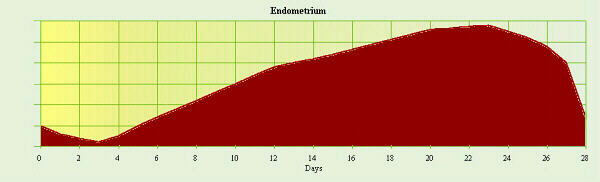
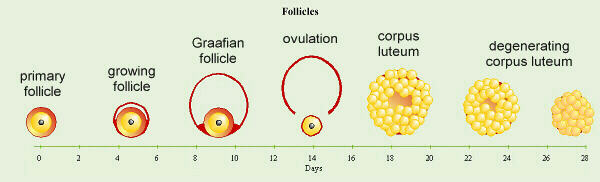
The first half of a woman’s cycle is the proliferative
phase (follicular phase), during which the endometrium starts to thicken.
The pituitary secretes FSH which causes (usually one) follicle to mature and
the ovaries to secrete estrogen. The ovarian estrogen secretion gradually
increases until just prior to ovulation. This gradually supresses secretion
of FSH and stimulates the hypothalamus to secrete a larger amount of GnRH
which, in turn, triggers the pituitary to secrete a burst of LH, causing
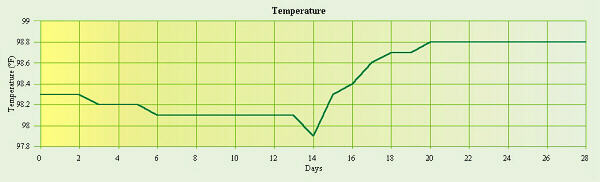
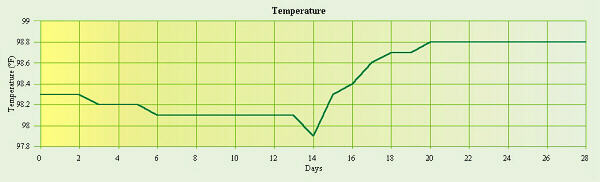
ovulation. During the proliferative phase, a woman’s body
temperature is low, perhaps as low as 98.0° F (36.7° C) or less. Sometimes
there is a slight rise near the end of the phase during the pre-ovulatory
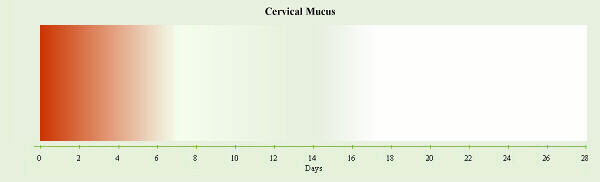
burst of LH before it dips again at ovulation. Throughout this phase, the
cervical mucus becomes progressively clearer and thinner.
On about day 14 of an average 28-day cycle, ovulation,
the rupture of the follicle and release of the egg, occurs in response to the
surge of LH. LH stimulates the remaining follicle cells to form a
corpus luteum
after ovulation. Often at ovulation there is a sharp drop in the woman’s
body temperature and her cervical mucus becomes very thin and clear and
forms “threads”. Interestingly, both the low body temperature and the
condition of the mucus are designed to prolong the life of and aid in the
mobility of sperm to increase the chances that the egg being released will
be fertilized.
The second half of the cycle is called the secretory
phase in the uterus and the luteal phase in the ovaries. The
endometrium continues to build up due to the secretion of progesterone (and
estrogen) by the corpus luteum, and this prepares the uterus for a possible
pregnancy. In case an egg has been fertilized, the growing embryo needs a
warmer environment to do well, so the body temperature rises to 98.6° F
(37.0° C) or higher. The cervical mucus becomes thick and paste-like,
blocking any more sperm from entering the uterus.
If an egg is not fertilized, as the corpus luteum deteriorates
at the end of a cycle, both estrogen and progesterone levels go very low.
In a pregnancy, implantation triggers hormone production that keeps the
corpus luteum secreting estrogen and progesterone for a while, but without
that, the corpus luteum disintegrates and stops secreting these hormones.
At this time, all of the hormone levels are low and decreasing. This
frequently causes the mood swings and other symptoms of premenstrual
syndrome (PMS), but PMS is also affected by diet, and large amounts of
salt, sugar, yeast, and/or caffeine can make things worse.
Throughout this discussion, the roles of the five hormones
that influence a woman’s menstrual cycle have been mentioned, but their
interactions are quite complex and involve both positive and negative
feedback loops. Reiterating the previous discussion specifically from the
point of view of the female hormone cycle will hopefully aid in better
understanding the roles played by these hormones.

Click on the animation to view it
again. When you see the “yes” and “no” choices, click one of those to
continue.
- GnRH from the hypothalamus stimulates
the pituitary to produce FSH.
- During the first part of pre-ovulatory
phase, the pituitary secretes low levels of FSH.
- FSH stimulates growth and maturation
of a follicle.
- As the follicle grows and matures, it
secretes estrogen in increasing amounts.
- The rising levels of estrogen exert
negative feedback on the pituitary to gradually lower the levels of
FSH.
- However, estrogen exerts a positive
feedback effect on the hypothalamus.
- Thus, just before ovulation, the
hypothalamus secretes a larger amount of releasing hormone which causes the
pituitary to secrete a burst of LH.
- The effect of this burst of LH on the
mature follicle causes it to rupture, release the egg, and start to form a
corpus luteum.
- After ovulation, LH stimulates the
corpus luteum to secrete progesterone and estrogen to prepare the uterus for
implantation.
- The rising/high levels of the
estrogen-progesterone combination in the blood exert a negative feedback
effect on the hypothalamus and pituitary, causing levels of LH to
decrease.
- As LH decreases, the corpus luteum
starts to disintegrate.
- Unless an embryo has implanted, near
the end of the post-ovulatory phase, without the stimulation of LH, the
corpus luteum stops producing estrogen and progesterone. Thus the
endometrium is no longer maintained and begins to deteriorate and is
shed.
- Thus, around the time a woman’s period
starts, all five hormones are at their lowest levels.
- However with the low estrogen and
progesterone levels, the hypothalamus can now begin again to secrete GnRH so
the cycle starts over.
- If an egg was fertilized, it begins
to divide as it travels down the Fallopian tube, and the blastocyst
that reaches the uterus is about 100 cells in size and ready to implant in
the endometrium. (Note that most “birth-control” pills work by prohibiting
this embryonic baby from implanting, so he/she dies. Thus, technically this
is a form of abortion. Depending on your personal point of view, you may or
may not consider this to be acceptable for you.)
- If implantation is successful, the
outer embryonic membrane, the chorion secretes human chorionic
gonadotropin (HCG) which maintains the corpus luteum during the first
trimester of pregnancy. Excess HCG is excreted in the woman’s urine,
thus many pregnancy tests test for the presence of HCG in urine.
- During the second trimester, the
placenta starts to secrete progesterone and stops HCG production. Because
of the lack of HCG, the corpus luteum, which is no longer needed,
degenerates. The endometrium is maintained by the hormones secreted by the
placenta.
Menopause:
Menopause, while technically, a woman’s last menstrual flow,
overall, is not a one-time incident, but rather, a process of change through
which her body goes. The age at which this change begins varies from
woman to woman. One book I read says if you’re experiencing “symptoms” that
prompt you to wonder, “Is this menopause?” the answer is, “Yes!” Interestingly,
studies have shown that in other cultures where menopause is regarded as a
normal stage in a woman’s life, where older women are respected for their
wisdom, and where, in general, aging is something desirable for the respect
and honor that it brings, women in those cultures do not experience nearly
as many (if any) of the bothersome symptoms experienced by women in this
country where menopause is treated like some kind of horrible disease,
and thus, something to be avoided at all costs (doesn’t work — can’t be done).
Those differences in symptoms exist despite the fact that hormone levels
in all the women were found to be similar. Thus, a woman’s attitude about
menopause can and does influence what, if any, symptoms she experiences
and the severity of those symptoms.
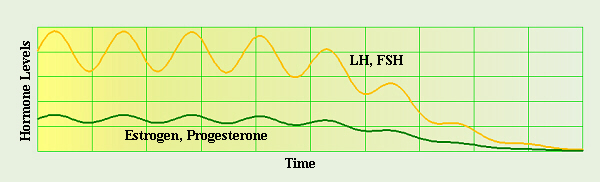
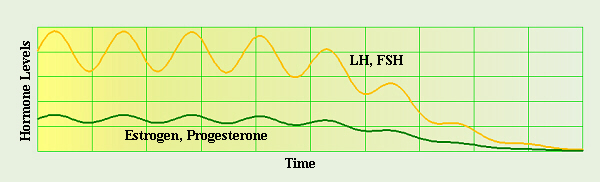
One leading hypothesis for what “causes” menopause is that
the ovaries run out of eggs, and thus, also follicles to turn into corpus
lutea, therefore also the estrogen and progesterone that would have been
produced by those follicles (similar to the green line, above). Initially
(for the first few years), in an attempt to increase the production of the
missing estrogen and progesterone, a negative feedback loop triggers the
hypothalamus to significantly increase production of LH and FSH (similar to
the yellow line, above). Since there are no more follicles to produce
estrogen in response, the large amounts of LH and FSH produced stimulate both
the ovaries and the adrenal glands to produce increased amounts of androgens
(testosterone), which the woman’s body can, then, convert to estrogen
(the same source of estrogen as in the body of a woman with
AIS
as discussed on previous Web pages), though that is far below the estrogen
level of a pre-menopausal woman. (Note: this graph is not totally accurate,
in that the process of change in the hormone levels would be spread out over
a number of years, not just a few cycles as shown here.)
Copulation/Sexual Intercourse/Coitus:
Copulation in most species of animals is preceded by
various courtship rituals which help insure that the most genetically
fit individuals pass on their genes. In humans, various activities including
“flirting” and “foreplay” lead up to and physiologically stimulate and
prepare the couple’s bodies for coitus, and in general, most women need
considerably more stimulation over a longer period of time than many men, to
physiologically prepare their bodies for sexual intercourse. Human mating
physiology includes four phases in the sexual response cycle.
- The excitement phase prepares
the vagina and penis for coitus or sexual intercourse.
Vasoconstriction, filling of the erectile tissue with blood occurs
because of increased flow in the arteries and constriction of the veins,
especially in the penis and clitoris, but also in the testes, ovaries,
female labia minora, and female breasts.
Myotonia,
increased muscle tension, causes erection of the nipples; tension in the arms,
legs, and other skeletal muscles; and sustained or rhythmic contractions of
the smooth (and skeletal) muscles.
- Many of these characteristics
continue into the plateau phase. In the female, the outer third of
the vagina becomes vasoconstricted, while the inner two thirds becomes slightly
expanded, and the uterus becomes elevated, all in preparation for receiving
sperm. Breathing and heart rates increase, not because of physical activity,
but because of stimualtion from the autonomic (sympathetic) nervous
system.
- Orgasm is rhythmic, involuntary
contractions of the reproductive structures/organs in both sexes. In the
male, this occurs in two stages: emission, in which the semen is
injected into the urethra; and ejaculation, in which the semen is
propelled into the woman’s vagina. A male normally has only one orgasm
(and some men may fall asleep during/after the resolution phase which follows).
In the female, orgasm involves the uterus and outer vagina but not the upper
two thirds of the vagina. Typically it is harder to stimulate a woman to
reach orgasm, and the man needs to take care to make sure the woman is ready
when he is. Women, however, can have multiple orgasms, and once aroused, are
often not ready to “quit” when, physiologically, the man’s body is progressing
to the resolution phase. Many women appreciate continued, gentle stimulation
after coitus.
- The resolution phase involves
a return to normal. During the resolution phase, vasoconstriction returns
to normal, the muscles relax, etc. While the changes that occur in most
structures occur within the first 5 min. after orgasm, loss of the male
erection often takes a little longer.
Fertilization and Embryonic and Fetal Development:
If the woman is just pre-ovulation or at ovulation,
conception, the start of a new person, of pregnancy, may occur.
Interestingly, there are some things a couple can do to increase their chances
of having a baby of a given sex. It has been found that sperm which contain
an X chromosome tend to live longer than Y sperm, so having intercourse a
couple days prior to ovulation increases the chances of a girl baby. On the
other hand, Y sperm swim faster than X sperm, so having intercourse right at
ovulation can increase the chances of a boy baby. As previously mentioned,
at the time of ovulation, a woman’s body temperature and cervical mucus are
“right” to help sperm survive. The contractions caused by orgasm and the
prostaglandins in semen help propel sperm up into the uterus, and from there,
up the Fallopian tubes. An “egg” is fertilized near the end of the Fallopian
tube, then finishes meiosis, the nuclei unite, and the embryo starts dividing
as it begins to travel to the uterus.
Recent work on human pheromones has turned up some interesting
effects they may have on pregnancy. It is not unusual in our busy society,
for a couple who desire a baby to keep track of where the woman is in her
cycle, and plan to have intercourse “at the right time,” yet, despite no
physical problems, many of these couples still fail to conceive. Recent
work on human pheromones suggests that this is not enough. Apparently the
woman’s body may need continued exposure to the man’s pheromones, such as
would be acheived by the close contact during coitus, several times a week
during the last two weeks of her cycle to make implantation more likely.
Again, evolutionarily, this would make sense in terms of signaling the
presence of a pair-bonded male who could provide her and her developing
child with enough food to survive the pregnancy. It would, then, make
sense that lack of continued pheromonal stimulation (as in when the couple
go back to their busy schedule until next month at the appointed time or in
a “one night stand”) would signal the absence of a male that could mean
increased hardship and lower chances of survival if pregnancy were to result.
However, in the interest of passing on one’s genes, evolutionarily, the
possibility of pregnancy is not totally ruled out, just diminished.
If an egg is fertilized, fertilization occurs in the far end
of the Fallopian tube near the ovary, and as the embryo travels down the
tube, cell division starts. By the time it reaches the uterus (about
a week later), it is a “hollow ball” or
blastocyst,
which has about 100 cells. The embryo, specifically the placenta, starts
producing hormones which prevent the corpus luteum from disintegrating, and
hormones from the corpus luteum maintain the endometrium until the placenta
is large enough to secrete more hormones on its own. Note that whereas
contraceptives, as their name suggests, prevent conception (union of
egg and sperm to form a new person), many of them also reduce the thickness
of the endometrium such that implantation is prohibited if an egg would
happen to “pop out” and unite with a sperm. Also, intrauterine
devices (IUDs) as well as “morning after” pills and some other drugs,
including Depo-Provera, work to prevent implantation of the week-old,
genetically-unique, growing embryo thereby causing it to die, and thus are
abortifacients.
When the embryo implants in the endometrium, it starts to form
the placenta. A human placenta attains the size of a dinner plate. The
placenta serves as the site of transfer of nutrients and wastes between the
maternal and fetal blood, and when large enough, it secretes hormones to
maintain the endometrium, thus the pregnancy. Keep in mind that the two
blood supplies do not come into contact with each other, but chemicals can
be passed back and forth.
In the first trimester (the first three months) of
pregnancy, most organogenesis, development of body organs occurs.
The baby’s heart starts beating at about four weeks (when the mother’s first
period is about two weeks late and she’s beginning to wonder if she might be
pregnant). Because so much critical growth and development takes place in
the first few weeks before she even knows she’s pregnant, it is very
important that she be well nourished (including vitamin supplements if needed,
especially folic acid to prevent neural tube defects) before she even tries
to get pregnant. By the end of the eighth week (when her second period is
two weeks overdue) all of the major body structures and organs of an adult
are present in at least rudimentary form, so the embryo is now called a
fetus. The rest of the time during pregnancy is mostly just growth.
Note that because of organogenesis, the first trimester is the time when the
growing baby is the most sensitive to adverse effects of drugs like
alcohol, tobacco, and caffeine, viruses like German measles, and lack of
necessary nutrients such as folacin. During the first trimester, the
placenta secretes HCG to maintain the corpus luteum which continues to
secrete the estrogen and especially progesterone needed to maintain the
endometrium. The cervical plug forms to protect the growing baby from
“foreign invaders”, and the woman’s breasts begin to enlarge in preparation
for lactation, or nursing. The level of HCG is so high in the
blood that some is excreted in the urine. Most pregnancy tests look for the
presence of HCG in urine. As the embryonic baby’s sex organs begin to
develop, (s)he starts with rudimentary forms of both male and female systems,
and only one set continues to develop while the other atrophies. Also the
initial development of external genitalia is similar and it can be difficult
to tell the sex of a baby early on.
In the second trimester growth occurs. The baby is
very active, and eventually these movements can be felt by the mother. The
baby can hear by the fourth month, and when born recognizes not only mom’s
voice, but also dad’s voice (if he’s around) and/or any other
frequently-heard, familiar sounds, perhaps including things like any musical
instruments the mother plays, etc. During this trimester, HCG production
declines and the corpus luteum stops producing progesterone as it deteriorates.
As this is happening, the placenta takes over and begins to secretes
progesterone itself to maintain the endometrium.
The third trimester is a time of rapid growth. The
baby tends to move less just because the uterus has become so crowded.
Estrogen levels in the mother’s blood reach their highest in the last weeks
of pregnancy, and as this increases, it triggers the formation of
oxytocin receptors in the uterus. Late in pregnancy, fetal cells
produce increasing amounts of oxytocin, another hormone, as does the
pituitary. Oxytocin is a powerful smooth muscle stimulant, and due to the
receptors which have formed in the uterus, causes uterine contractions. The
high estrogen levels also stimulate the placenta to make prostaglandins
(similar to those that cause “cramps”) that also stimulate contractions. The
hormonal induction of labor is a positive feedback loop. Oxytocin and the
prostaglandins cause uterine contractions that, in turn, stimulate the
release of more oxytocin and prostaglandins. This is partially due to
pressure of the baby’s head against the cervix that both dilates the
cervix and acts on cervical nerve endings to stimulate the production of
oxytocin, which causes stronger contractions that cause the baby’s head to
be pressed more strongly against the cervix, etc.
Probably some of the most famous pictures of human embryos
and fetuses have been taken by a Swedish photographer named
Lennart Nilsson.
Labor and Delivery:
There are three stages in the birth process, including:
- the dilation of the cervix,
which lasts from the onset of labor until the cervix reaches its full
diameter of about 10 cm, and is the longest stage, often lasting 6 to 12 hr
or longer,
- the expulsion stage, the time
(about 20 min to 1 hr) from full dilation until delivery, during which,
strong contractions about 1 min each occur every 2 to 3 min, and the mother
feels an increasing urge to push until the baby is forced down, into the
vagina, and out, and
- the delivery of the placenta
which usually occurs within 15 min of the delivery of the baby.
When the baby is born, much of his/her blood is still
circulating to/from the placenta, and as (s)he begins to breath, that blood
is naturally brought back into the body, aided by the pulsating of the
umbilical cord. After the baby is born, the umbilical cord will continue to
pulsate for a few minutes to return as much blood as possible from the
placenta into the baby’s body. For optimum health of the baby, it is
important that as much of the baby’s blood as possible be out of the placenta
and into the baby’s body before the cord is cut, thus the person doing this
should wait until the cord stops pulsating before clamping and
cutting it. Many medical staff people try to rush through this procedure
and cut the cord too soon, often clamping and cutting the umbilical cord,
before the placenta is even delivered.
After birth, decreasing progesterone and estrogen and
increasing oxytocin help reduce the uterus to its normal size. It has been
found that laying the baby on the mother’s abdomen immediately after birth
will stimulate the production of oxytocin, helping shrink the uterus faster.
The baby’s sucking on the mother’s nipples stimulates nerve endings that
also stimulate the production of oxytocin, so immediate
postpartum
nursing can also help return uterus to proper size.
The hormones oxytocin and prolactin trigger the
production of milk. While these are present initially in quantities
sufficient to begin lactation, the baby’s sucking triggers further
release of these hormones, in yet another positive feedback loop. At first,
colostrum is produced. This nutrient-rich substance contains lots of
antibodies, etc. important to the baby’s health for the first few days and
it’s very important that the baby have the benefit of this nutrition. Also,
nursing is important in the bonding process (a human baby imprints on the
smell of his/her mother’s nipples), and for that reason, too, it’s very
important to let a baby nurse immediately after birth.
Instinctively, when a newborn is first trying to nurse, (s)he will turn
his/her mouth toward anything that brushes his/her cheek. Frequently, in
hospital setting, well-meaning nurses trying to “help” can actually distract
and confuse the baby by touching the baby’s face, thus making it harder for
the baby to find the nipple. In contrast, brushing the baby’s cheek with
the nipple will cause the baby to turn toward it. About 2 to 3 days after
the birth, the mother’s real milk will begin to be produced. This is a
specially-designed food source that exactly matches the nutritional needs of
a baby, thus every effort should be made to make use of mother’s milk rather
than artificial substitutes which often are nutritionally lacking.
Contraception/Birth Control and Abortion:
For couples who are trying to avoid creating a baby, a number
of birth control methods that prevent fertilization (contraceptives)
are available, but not all methods of birth control fit into that category.
In one method of “natural” birth control, the woman must have very regular,
predictable cycles and must keep a very accurate, daily record of her body
temperature (first thing in the morning before getting out of bed) and
condition of her cervical mucus in order to determine when ovulation is
occurring. The couple must, then, cooperate in being willing to
forego a few minutes of pleasure within several days of ovulation, and instead,
show their love for each other in some other way, in the interest of
building a strong, long-term, loving relationship.
Since many women’s cycles are not that predictable and/or many women do not
wish to keep such detailed records and/or many couples would rather not have
to consult a calendar, a variety of other methods of preventing ovulation or
preventing sperm from reaching the egg are available.
Some of the hormone pills prevent ovulation (but many of those also prevent
implantation), and many of the barrier methods attempt to prevent sperm from
getting up into the uterus, either by introducing a physical barrier between
the penis and the uterus (cervical cap, diaphragm, condom) or by killing the
sperm (spermicidal chemicals inserted into the vagina).
However, none of these methods is a substitute for willpower and personal
responsibility, and will not prevent conception if the people involved do
not choose to discipline themselves to “make it work.” If a barrier or
foam is neglected or used improperly or if a woman doesn’t take the pills on
schedule, a baby is a likely outcome.
Birth control methods that permanently make reproduction impossible are called
sterilization, and include things like vasectomy, tubal ligation, and
hysterectomy.
As mentioned above, some birth control methods like IUDs and
many drugs prevent an already-fertilized and growing embryo baby from
implanting in the uterus, thus are abortifacients, agents that cause
abortions. RU-486 is specifically meant to kill an unborn baby, and must be
taken in conjunction with other drugs that cause uterine contractions to
expel the dead baby. According to patient literature which some of my
female students received along with Depo-Provera injections, this drug works
by thinning the endometrium of the woman’s uterus so that when/if a
week-old blastocyst-stage embryo reaches her uterus, it will have no place to
implant, and will, thus, die. While some people feel that abortion should
legally be available as a means of correcting “mistakes,” it is not a
contraceptive and should not be routinely used as such. Legal or not,
abortion is not a substitute for personal willpower and responsibility for
one’s own actions.
In early abortions, a suction device is used to dismember and remove the
baby in pieces. In mid-term abortions, special tongs are used to dismember
the baby and remove the arms, legs, head, genitalia, torso, etc. in pieces.
In late-term abortions, some of the amniotic fluid is replaced with a strong
salt solution to try to burn/poison/kill the baby, and the woman is then
given drugs to induce labor — a number of these babies have been born alive
and with bad chemical burns, and there have been cases where such babies are
just dumped into a bucket and left there until they die. In late-term,
“partial birth” abortions, the baby is manipulated into the breech birth
position (harder and more dangerous for the mother), then labor is induced.
At the end of the delivery, as the mother’s uterus is contracting to try
to finish getting the baby out, the baby’s head is held inside the mother’s
vagina (so the birth isn’t “official”) while a suction device is inserted at
the top of the baby’s spine to suck out and remove his/her brain. When the
baby is dead, the head is allowed to be born.
Numerous studies have shown that women who go through these procedures often
suffer from depression, sometimes severe, as a result. Studies have even
found that years later, often without consciously realizing the cause, many
of these women suffer depression especially on the anniversary of the date
they had the abortion and/or on what would have been their child’s
birthday.
If you would like to watch an actual abortion to see what
goes on in a mid-term abortion, here are three links to copies of the
movie “Eclipse of Reason” that people have uploaded to YouTube:
http://www.youtube.com/watch?v=QgCMEeaWjZA
http://www.youtube.com/watch?v=_nff8I2FVnI
http://www.youtube.com/watch?v=s5ILndK3aDg
Be forewarned before watching that this movie can be VERY upsetting.
DO NOT LET YOUNG CHILDREN WATCH THIS MOVIE!
The only totally effective method of preventing making a baby
(short of sterilization) is abstinence, yet in our culture, we’re bringing
up a whole generation of young people who are being taught that they couldn’t
possibly be expected to have the personal willpower and responsibility for
their actions to make that work. In previous generations when young people
were taught that they were capable of abstinance and were expected to abstain
from sexual intercourse until marriage, the rates of teen-age pregnancies
among unwed mothers were much lower (as were the rates of STDs).
Sexually-Transmitted Diseases
A number of sexually transmitted diseases (STDs) are
caught/spread by having sexual intercourse with multiple partners, thus are
easily avoided if a person so chooses. Some of these diseases are caused by
viruses, while others are bacterial in origin. For example, “genital warts,”
or human papiloma virus (HPV) is spread by sexual contact or by lying, naked,
on an unsterilized tanning bed. HPV has been associated with cervical
cancer in women, often necessitating a hysterectomy, perhaps at a
young-enough age to preclude any opportunity of having children.
One interesting aspect of this is that while our government
has been telling people that use of condoms will prevent STDs, current
research indicates that’s not entirely true. The latex of which condoms are
made, just like any chemical, has pores or holes in between the molecules of
which it is made. These holes are small enough that relatively large sperm
cells are larger than the holes, so usually don’t get through. However,
viruses like the AIDS virus are several powers of 10 smaller in size than a
“large” sperm cell, and are smaller than the size of the holes in the latex,
thus can go through them and infect someone! Since the holes in the latex
are “twisted” as they go through the latex, and not exactly lined up or
a “straight shot” going through them, that does somewhat lessen the chance
that an AIDS (or other) virus can find its way through. Thus, while use of
condoms may reduce the chances of getting AIDS or some other virus,
they do not prevent these diseases.
Other than unusual cases like hemophiliacs who need blood
transfusions, the vast majority of people can control their chances of
contracting AIDS if they choose to do so. Your chances of being exposed to
AIDS are directly dependent on your lifestyle. If you choose to have sexual
intercourse with many partners and have no idea with whom else they’ve had
intercourse, it is very likely that you will get AIDS. If you choose
to save sexual intercourse for a special, lifelong commitment to one partner
who feels the same way, and you’re both the only ones you’ve ever had sex
with (and neither of you does IV drugs, etc.), neither of you will be
exposed to AIDS.
Also, note that the relatively-thicker walls of a woman’s
vagina were designed to take the physical stress of sexual intercourse,
while the relatively-thinner walls of a person’s rectum were not. Thus,
“anal sex” frequently causes tears in the walls of the rectum which, if
one’s partner is infected with an STD, can serve as entry sites for that
infection into the other partner. The tears from anal sex can significantly
damage the rectum, which may necessitate painful, corrective surgery to
“fix” accumulated rectal damage. If the person’s immune system has been
“destroyed” by an HIV infection, the healing process following such surgery
can be complicated by increased chances of infection.
References:
Berkow, Robert, ed. 1987. The Merck Manual. 15th Ed. Merck, Sharp & Dohme, Rahway, NJ.
Berkow, Robert, ed. 1999. The Merck Manual. 17th Ed. Merck, Sharp & Dohme, Rahway, NJ.
Borror, Donald J. 1960. Dictionary of Root Words and Combining Forms. Mayfield Publ. Co.
Campbell, Neil A., Lawrence G. Mitchell, Jane B. Reece. 1999. Biology, 5th Ed. Benjamin/Cummings Publ. Co., Inc. Menlo Park, CA. (plus earlier editions)
Campbell, Neil A., Lawrence G. Mitchell, Jane B. Reece. 1999. Biology: Concepts and Connections, 3rd Ed. Benjamin/Cummings Publ. Co., Inc. Menlo Park, CA. (plus earlier editions)
Marchuk, William N. 1992. A Life Science Lexicon. Wm. C. Brown Publishers, Dubuque, IA.
Murray, Michael T. 1994. Menopause. Prima Publ. Rocklin, CA.
Weed, Susun S. 1992.Menopausal Years the Wise Soman Way. Ash Tree Publ. Woodstock, NY.
http://www.pbs.org/wgbh/evolution/library/01/6/l_016_08.html (information on the “sweaty t-shirt” experiment)
http://en.wikipedia.org/wiki/Claus_Wedekind (information on the “sweaty t-shirt” experiment)
Copyright © 1996 by J. Stein Carter. All rights reserved.
This page has been accessed  times since 14 Mar 2001.
times since 14 Mar 2001.